Cytomegalovirus Infection
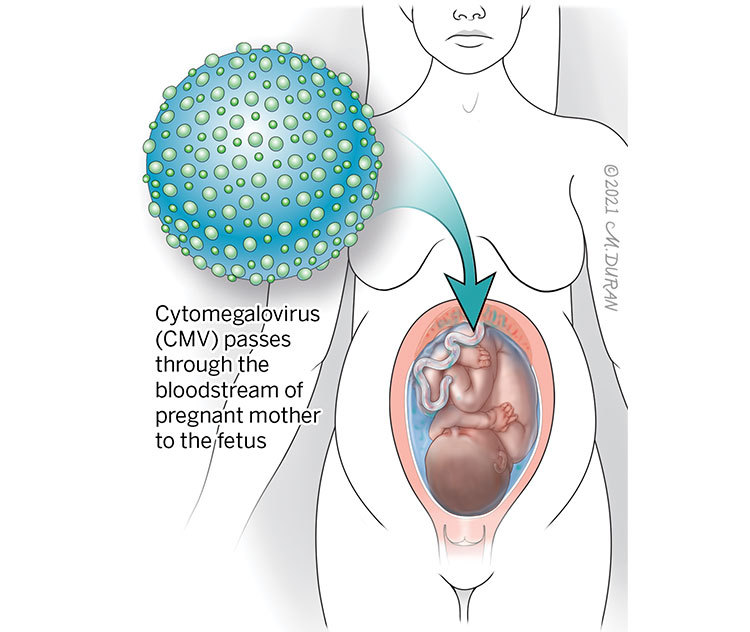
Cytomegalovirus (CMV) is a very common viral infection that is related to a type of herpes virus and affects people of all ages. Approximately 1 to 4 in 100 women contract CMV during pregnancy. If a woman catches CMV during pregnancy, the pregnant mother has a 1 in 3 (33%) chance of passing CMV to the unborn baby. Although extremely rare, CMV can cause complications for an unborn baby.
About Cytomegalovirus Infection
You can contract CMV if you come into prolonged contact with infected bodily fluids, such as urine, saliva, mucus, blood, feces, or semen. The most common risk factor for CMV in pregnancy is contact with young children in the daycare setting as the virus is commonly found in the saliva and urine of young children (particularly between the ages of 1 to 3) and frequently spreads among toddlers at daycare centers. Much like other members of the herpes virus family, a prior CMV infection can “reactivate” and return.
A primary CMV infection occurs when a pregnant woman gets infected for the first time. A recurrent CMV infection occurs when there has been a prior infection and the virus has returned to its active state. CMV can be passed from the pregnant mother’s blood to the baby through the placenta at any time during pregnancy whether the pregnant mother is infected for the first time or a prior CMV infection has reactivated. If you catch CMV during pregnancy, it very rarely causes complications for an unborn baby. However, it’s important to be monitored by your doctor, because for some babies, CMV can cause serious health problems.
Symptoms of Cytomegalovirus Infection
CMV often comes and goes without any obvious symptoms; however, some symptoms may appear.
Symptoms of CMV infection may include:
- Constant, persistent fatigue
- Fever that lasts a few days
- Sore throat
- Swollen glands
These symptoms usually resolve on their own within approximately three weeks.
Complications Associated With Cytomegalovirus Infection
CMV is not associated with any health risks for the pregnant mother. Almost all severe CMV infections diagnosed in the fetus are the result of the pregnant mother contracting a CMV infection in the first 12 weeks of the pregnancy. Approximately 33% of all cases in which the pregnant mother has contracted a primary CMV infection during pregnancy will result in the passing of the virus through the placenta and into the bloodstream of the fetus. In some cases, the fetus will not exhibit any signs of the infection on ultrasound. In other cases, a more serious problem may occur in the fetus known as hydrops. In this scenario, fluid can build up in the abdomen (ascites), around the lungs (pleural effusions), around the heart (pericardial effusion), and in the skin (subcutaneous edema). The placenta can also become thick with fluid (placentomegaly) and there can be excess fluid in the sac surrounding the fetus (polyhydramnios). If left untreated, hydrops can become a sign of the impending death of the fetus.
Diagnosing Cytomegalovirus Infection
Fetal CMV infection is more commonly suspected when specific abnormal findings appear on ultrasound.
Signs of fetal CMV may include:
- A head that appears small in size (microcephaly)
- Calcifications (abnormal deposits of calcium) in the fetal head near the fluid-filled compartments (ventricles)
- Echogenic bowel
- Extra fluid in the fetal abdomen (ascites)
- Fetus appears to be small in size (intrauterine growth restriction)
- Increased fluid in the compartments in the brain (ventriculomegaly)
- Thickened placenta
If fluid is present in other areas of the fetus, such as around the lungs (pleural effusion), around the heart (pericardial effusion), or in the skin (edema), then the overall condition is known as hydrops fetalis.
An immunoglobulin blood test can be performed on the pregnant mother to measure the level and types of antibodies in the blood, which may indicate the presence of a CMV infection.
Antibodies that may indicate the presence of a CMV infection:
- Immunoglobulin M (IgM): If positive, may indicate a new infection.
- Immunoglobulin G (IgG): If positive, may indicate a new or old infection. If negative, the pregnant mother is still susceptible to contracting a CMV infection.
- An Immunoglobulin G (IgG) avidity test can help determine if the IgG represents a recent infection (low avidity) or a prior infection (high avidity).
If your test results are positive, your fetal medicine specialist may suggest that an amniocentesis be performed using a test known as a polymerase chain reaction (PCR) to determine if a CMV infection is present. During this procedure, a needle is placed into the uterus using ultrasound for guidance. The needle is then connected to a tube and a sample of the fluid found around the fetus is extracted. If the results of this test are positive, then the fetus is infected with CMV. On rare occasions, the results of the test can be negative even though the newborn is diagnosed with CMV at birth. This usually occurs when the amniocentesis is performed too soon after the pregnant mother has contracted the CMV infection. Due to this, an amniocentesis is typically scheduled once a minimum of two months has passed since the mother became infected and the fetus has reached a minimum of 17 weeks (4 months, 1 week) of gestation.
Pregnancy With Cytomegalovirus Infection
If a fetus develops excess fluid in the sac surrounding the fetus (polyhydramnios), this can lead to maternal discomfort and, in some cases, problems with maternal breathing. In these cases, the fluid can be temporarily drained from the sac around the fetus through a procedure known as amnioreduction. During this procedure, a needle is placed into the uterus using ultrasound for guidance. The needle is then connected to a tube and the excess fluid is drained over a 20- to 30-minute period of time.
If a fetus develops both hydrops and placentomegaly, a condition known as mirror syndrome can occur in the pregnant mother. In this situation, the mother begins to mirror the findings in her fetus in which extreme retention of fluid and breathing difficulties arise due to fluid buildup in her lungs. High blood pressure can also occur and become a complication. The only treatment for maternal mirror syndrome is delivery of the fetus. After delivery, the mother’s symptoms will resolve over several days.
After the initial ultrasound evaluation, you will likely be scheduled for fetal magnetic resonance imaging (MRI). A fetal MRI is similar to a CT scan but does not involve X-rays or radiation. Instead, a special magnet is used to produce images of the structures in the fetus that cannot be seen easily with ultrasound. A fetal MRI is safe for both you and your baby. You will likely need ultrasounds every 3 to 4 weeks to monitor the overall growth of your baby, examine any changes or other findings in the brain, and to determine whether your baby has developed hydrops. You may also be scheduled to meet with a pediatric infectious disease specialist that has knowledge about treating CMV in newborns.
A vaginal delivery is safe for babies with CMV. Most women with a baby in utero with CMV will be allowed to go into spontaneous labor near their due date. In some cases, you may be required to delivery earlier if your baby shows evidence of poor growth along with decreased fetal movement.
Treating Cytomegalovirus Infection
Treating the pregnant mother with a high dose of Valtrex® , a drug used to treat genital herpes, has been associated with a 50% increase in the chance of the newborn not showing any signs of CMV. If you and your fetal medicine specialist decide to use this drug, blood tests may be performed occasionally to monitor the development of any side-effects.
In approximately 90% of fetal infections with CMV, the newborn is asymptomatic (does not show signs of infection). 85% of these newborns have a normal outcome. In 15% of cases, developmental problems can occur, most often involving hearing loss. This hearing loss may be detected soon after birth or it may occur later in life (during the first 4 to 6 years of age). Approximately 5% of babies born with CMV will show signs of very severe infection and may die in the nursery from their disease. In some cases, babies born with CMV will suffer more severe neurologic problems, including seizures, development delays, cerebral palsy, and loss of vision.
Evaluation After Birth
After birth, your baby will undergo testing of their urine or saliva to determine if a CMV infection is present. Your baby’s blood will be drawn to examine blood counts and to assess for liver problems. A hearing test will be performed (which is required by state law for all newborns), and both an ultrasound of the baby’s abdomen and an MRI of the baby’s head may also be ordered. Your baby will likely be evaluated by a pediatric infectious disease expert who may want to place the baby on a special antiviral treatment drug known as ganciclovir.
Care Team Approach
The Comprehensive Fetal Care Center, a clinical partnership between Dell Children's Medical Center and UT Health Austin, takes a multidisciplinary approach to your child’s care. This means you and your child will benefit from the expertise of multiple specialists across a variety of disciplines. Your care team will include fetal medicine specialists, obstetricians, neonatologists, sonographers, palliative care providers, fetal center advanced practice providers, fetal center nurse coordinators, genetic counselors, and more, who work together to provide unparalleled care for patients every step of the way. We collaborate with our colleagues at The University of Texas at Austin and the Dell Medical School to utilize the latest research, diagnostic, and treatment techniques, allowing us to identify new therapies to improve treatment outcomes. We are committed to communicating and coordinating your care with your other healthcare providers to ensure that we are providing you with comprehensive, whole-person care.
Learn More About Your Care Team

Comprehensive Fetal Care Center
Dell Children's Specialty Pavilion
4910 Mueller Blvd. Austin, TX 78723
1-512-324-0040
Get Directions