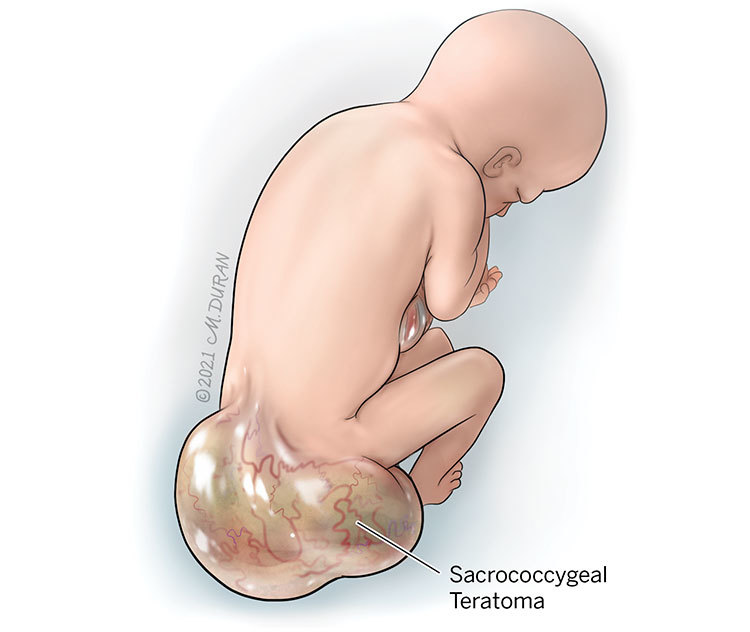
Sacrococcygeal Teratoma
A sacrococcygeal teratoma (SCT) is a tumor that develops before birth at the base of a baby’s spine near the tailbone (coccyx). SCTs are relatively rare and occur in approximately 1 out of every 23,000 to approximately 1 out every 40,000 pregnancies worldwide.
About Sacrococcygeal Teratoma
All human embryos begin with germ cells, which give rise to three major cell lines of an embryo: ectoderm, mesoderm, and endoderm cells. Each of these cell lines form its own set of tissues and organs as the embryo develops into a fetus. An SCT is a tumor growth at the lower spine of a fetus or newborn that contains cells from all three cell lines. The growth is thought to arise from the area where germ cells persist (Hensen’s node), which is located near the coccyx at the lower end of the spine. In most cases, the SCT is not cancerous; however, in rare cases, cells that are considered a form of cancer can be present. While developing an SCT is four times more common in female fetuses than in male fetuses, malignancy (cancerous cells) is more common in male fetuses. The different types of SCTs are classified according to the location of the tumor.
Types of SCTs include:
- Type I sacrococcygeal teratomas are completely located outside of the fetus.
- Type II sacrococcygeal teratomas have some tissue located on the outside of the fetus and some tissue located on the inside the lower body of the fetus.
- Type III sacrococcygeal teratomas have a larger component of the tumor located inside the lower body of the fetus and a smaller portion located on the outside of the fetus.
- Type IV sacrococcygeal teratomas are completely located inside the fetus.
Symptoms of Sacrococcygeal Teratoma
The symptoms that occur with sacrococcygeal teratomas vary widely depending upon the size and specific location of the tumor. Small tumors are often asymptomatic (do not cause any symptoms) and can usually be removed surgically after birth without difficulty. However, larger sacrococcygeal tumors can cause a variety of complications before and after birth.
Causes of Sacrococcygeal Teratoma
The cause of an SCT remains unknown. Similar teratomas can occur in the fetal neck and some in adult ovaries.
Complications Associated With Sacrococcygeal Teratoma
Although rare, problems with other organs can arise in a fetus with SCT, which is why a complete assessment of the fetal anatomy should be undertaken by an experienced physician using ultrasound. A fetal MRI may also be useful in assessing the fetal anatomy. The presence of chromosomal abnormalities in fetuses with an SCT are also rare.
SCTs usually have a significant amount of blood vessels that feed into them. This can put a strain on the fetal heart and cause high output heart failure. Additionally, bleeding can occur into the SCT, causing fetal anemia, which places further strain on the fetal heart.
In some cases, the fetus may develop hydrops in which fluid builds up in the abdomen (ascites), around the lungs (pleural effusions), around the heart (pericardial effusion), and in the skin (subcutaneous edema). The placenta can also become thick with fluid (placentomegaly) and there can be excess fluid in the sac surrounding the fetus (polyhydramnios). If left untreated, hydrops can become a sign of the impending death of the fetus.
In rare cases, the internal portion of the SCT can compress the fetal bladder, leading to a blockage of urine and decreased fluid in the sac surrounding the fetus (oligohydramnios).
Approximately 50% of fetuses with an SCT will survive. Large SCTs and SCTs that are mostly solid in nature are more often associated with poor fetal outcomes.
Diagnosing Sacrococcygeal Teratoma
SCTs are usually found at the time of an anatomy ultrasound at around 20 weeks (5 months) of gestation. They appear as a mass with solid tissue and fluid filled spaces at the lower end of the fetal spine. SCTs are often confused with spina bifida which can occur in the same location in the fetus.
Pregnancy With Sacrococcygeal Teratoma
If a fetus develops excess fluid in the sac surrounding the fetus (polyhydramnios), this can lead to maternal discomfort and, in some cases, problems with maternal breathing. In these cases, the fluid can be temporarily drained from the sac around the fetus through a procedure known as amnioreduction. During this procedure, a needle is placed into the uterus using ultrasound for guidance. The needle is then connected to a tube and the excess fluid is drained over a 20- to 30-minute period of time.
If a fetus develops both hydrops and placentomegaly, a condition known as mirror syndrome can occur in the pregnant mother. In this situation, the mother begins to mirror the findings in her fetus in which extreme retention of fluid and breathing difficulties arise due to fluid buildup in her lungs. High blood pressure can also occur and become a complication. The only treatment for maternal mirror syndrome is delivery of the fetus. After delivery, the mother’s symptoms will resolve over several days.
After the initial evaluation, you will be scheduled for ultrasounds every 1 to 2 weeks to assess for evidence of heart failure and hydrops. A fetal echocardiogram may also be scheduled on a regular basis to more accurately measure the actual fetal cardiac output. You will likely also be scheduled for a prenatal consult with a pediatric surgeon who will remove the SCT after your baby is born.
Treating Sacrococcygeal Teratoma
There are small case series that have been reported where fetuses have undergone open fetal surgery to resect part of the tumor. The fetus is then allowed to remain in the uterus in the hope that the cardiac failure will resolve. Only about 40% of these cases have been successful as premature delivery often complicates the recovery period after the surgery.
In rare cases where the fetus is very premature, fetal medicine specialists have attempted to stop the blood flow to the SCT using laser needle procedures or by injecting medications. These cases have rarely been successful due to the many blood vessels that are present in these tumors.
After 28 weeks (7 months) of gestation, premature delivery by c-section seems to be associated with the best outcome since the fetus can be stabilized in the neonatal intensive care unit and then the SCT can be removed through surgery. Fetuses with SCT are usually delivered by c-section unless the tumor is very small. Typically, a decision is made for a premature delivery. After delivery, the infant will be admitted to the neonatal intensive care unit.
Evaluation After Birth
After birth, once the neonatal team feels that the baby is stable, pediatric surgeons will remove both the tumor and the coccyx in attempt to prevent the tumor from returning. Once the tumor has been resected, doctors will look at tissue slices under the microscope to see if there are any abnormal cancerous cells present. If such cells are present, the baby may need to undergo treatment with chemotherapy. This therapy is generally very successful in treating these cells.
Babies with SCT are usually assessed by pediatric surgeons who conduct weekly to monthly exams and blood tests for the first year of the baby’s life and then yearly thereafter until the baby reaches 5 years of age. Imaging studies using MRI or ultrasound may also occur. Some babies require additional surgeries to improve the cosmetic look at the resection site.
Long-term studies of babies after SCT removal reveal that the majority do not experience any additional problems. A higher incidence of constipation, problems with bladder emptying, and kidney infections have been reported. Large tumors and tumors with malignant (cancerous) elements are more likely to be associated with these issues.
Care Team Approach
The Comprehensive Fetal Care Center, a clinical partnership between Dell Children's Medical Center and UT Health Austin, takes a multidisciplinary approach to your child’s care. This means you and your child will benefit from the expertise of multiple specialists across a variety of disciplines. Your care team will include fetal medicine specialists, obstetricians, neonatologists, sonographers, palliative care providers, fetal center advanced practice providers, fetal center nurse coordinators, genetic counselors, and more, who work together to provide unparalleled care for patients every step of the way. We collaborate with our colleagues at The University of Texas at Austin and the Dell Medical School to utilize the latest research, diagnostic, and treatment techniques, allowing us to identify new therapies to improve treatment outcomes. We are committed to communicating and coordinating your care with your other healthcare providers to ensure that we are providing you with comprehensive, whole-person care.
Learn More About Your Care Team

Comprehensive Fetal Care Center
Dell Children's Specialty Pavilion
4910 Mueller Blvd. Austin, TX 78723
1-512-324-0040
Get Directions